Seroprevalence in Mumbai: An Interview with Anup Malani
Editor-In-Chief Jay Bhattacharya interviews Professor Anup Malani about the effects of COVID-19 lockdowns in slums compared to more affluent areas of the city
Can you tell us a bit more about your background, and in particular, how you came to run a study of disease seroprevalence in Mumbai in July 2020?
I am, by training, an economist and a lawyer. One of the first topics I worked on after graduating was the dynamics of infectious disease. As I thought more about control of infectious disease, I realized two problems. First, countries and people do not have an incentive to report disease for fear of trade sanctions or quarantines. Thus, non-pharmaceutical infections are self-limiting because they make people hide information. Second, how people acquire information can affect disease requirements. Working with Dan Bennett (USC), I studied SARS in Taiwan. We documented that both news reports and rumours about infections triggered precautionary behaviour, specifically hospital avoidance, because people thought that the disease was spread at hospitals, which in turn may have accelerated the end of the epidemic. More recently, I began to study viral evolution. Working with Sarah Cobey, I examined how flu vaccination affects the evolution of flu, a topic that bears some resemblance to the problem of new variants of COVID-19. We were in the middle of revising our paper with the pandemic hit.
In parallel with my work on infectious disease, I was working on evaluating health insurance programs (via randomized controlled trials) in India and learning about the economics of slums via a large ethnographic project across ten cities in India. While doing this work, I met Reuben Abraham, head of IDFC Institute, who was also dedicated to improving state capacity.
When COVID hit India, Reuben and I had the idea to start a task force bringing together folks from the private sector (CEOs, heads of civil society, local experts) and retired bureaucrats to support the government in its COVID response in any way we could. Finally, noting the large chasm between the modelling resources available to the US/UK and India, I started an academic group with the help of folks like Jon Gruber, Luis Bettencourt, and Ashish Goel.
At first, the IDFC task force focused on logistics and communications during the national lockdown in March. The academic task force focused on epidemiological modelling of the epidemic, which we did for the centre and then some states. But we quickly realized the shortage of testing was a hurdle to policymaking. Through Reuben I met Manoj Mohanan from Duke and Anu Acharya, the CEO at Mapmygenome, a private testing company. We have been working on testing across a number of states from Assam, Andhra Pradesh and Goa to Bihar, Mumbai and Karnataka. A lot of it was advisory work, helping states plan population-level testing and helping analyze data even from non-systematic surveillance.
But one of our first projects was an effort to test for COVID in Mumbai slums. Manoj and I feared that, because of the population density in slums, that COVID would spread most quickly there. Working with a team of local scholars (Ullas Kolthur, Jayanti Shastri, Gagandeep Kang, and Sandeep Juneja, Sachee Agarwal, and Rajesh Jain), local NGOs and think tanks (led by Gayatri Lobo and Sofia Imad), and with the support of far-sighted local officials (Daxa Shah), Manoj and I were able to help conduct a population-representative serological survey of slum residents in wards from each of the three regions of the city in July and again in August 2020.
What exactly does seroprevalence mean?
Seroprevalence is the fraction of a population that has antibodies to SARS-CoV-2. To explain this, it is helpful to understand the immune response to the virus. When a person is infected, the body attempts to attack the virus. To do so, it must first identify and locate copies of the virus. To do so, it uses antibodies, which are pieces of protein that latch onto the virus and in turn signal the body’s white blood cells to attack what they are latched on to. These antibodies can also neutralize the virus by blocking its ability to enter human cells and replicate. For a person who does not already have immunity to virus, it takes time for the body to develop and produce antibodies that identify and neutralize the SARS-CoV-2 virus. But after it does and those antibodies help clear the infection, the antibodies may linger in the bloodstream for some time. If we draw a person’s blood and find antibodies that can latch onto a bit of protein that look like SARS-CoV-2, we can conclude that the individual had battled SARS-CoV-2 sometime in the past. If we take blood draws from a large number of people, we can calculate the fraction that has antibodies; this fraction is called the seropositivity rate. If the pool of blood samples is a representative draw from the population, the fraction of seropositive in the sample gives us an unbiased estimate of the fraction of the population that is seropositive, i.e. tests positive for antibodies.
Why is it important, from a scientific and policy perspective, to know the seroprevalence of COVID-19 in different places?
The reason it is important to know seroprevalence is that it gives us a sense of how many people were previously infected by COVID-19 and might now be immune to harm from future infection. It can also help us determine what harm COVID-19 does to people who are not immune. If we have a count of how many people died from COVID and we know the number of people previously infected with COVID, then we can calculate what is called the infection fatality rate (IFR), or the probability of dying if you have COVID. Seroprevalence estimates from a representative sample of donors can help us determine how many people were infected.
Using seroprevalence to determine the number infected is better than using the number of people with confirmed RT-PCR or rapid antigen tests. The latter tests measure whether the donor is currently infected, not whether she was infected in the past. Therefore, they tend to undercount the number of people who were ever infected. A measure of the fatality rate from COVID-19 based on the number of deaths among the people currently infected is called the case fatality rate (CFR). The problem with the case fatality rate is that it tends to overestimate the infection fatality rate, the harm from the infection because governments do not test enough, typically because testing is costly or unavailable. Another problem with tests for current infection is that they are usually done only if a person is symptomatic or had recent contact with someone who is symptomatic. But many COVID-19 infections, perhaps over 90% in India, produce no symptoms, i.e., are asymptomatic. That means that those who are tested are more likely to have health problems from COVID, including death. So CFR, which, if anything, measures the fatality rate among symptomatic infections, is typically much greater than IFR.
The benefit of knowing the harm from COVID is that we can use it to inform infection control policy. We have learned that COVID-19 has a much higher IFR among older individuals than younger ones. This, in turn, can tell us how to allocate scarce COVID vaccines: target the elderly to maximize health benefits. It can also help us determine the net benefit from different non-pharmaceutical interventions, which may have their own costs, especially for the poor. With high IFR, we can be more confident that lockdowns are helpful. With low IFR, they might not be.
What was life like in normal times (pre-pandemic) for people living in the Dharavi slums in Mumbai? What are the typical living arrangements like for people living there?
I am going to tell you about slums in general, not just in Dharavi. Because Dharavi has gotten so much media attention, it has also benefited from a lot of NGO and charitable aid. That, in turn, has rendered it a better-off neighbourhood than other slums.
To understand the physical structure of slums, one has to understand urbanization and housing markets in cities. People come from rural India to cities because cities are vibrant places that generate jobs, opportunities for educating children, and escape from the traditional, caste-centred social structure in villages. When people come to cities for work, they need housing. Unfortunately, cities in India, like those in the US, put up many obstacles to housing construction. Because there are so many people looking for legal housing and a regulatory drag on the number of formal homes, the price of these homes is quite high. Certainly much higher than new migrants, especially poor migrants, can afford.
So these new migrants, on the bottom rung of the city’s economic ladder, find any open space they can and build a make-shift home. They have no legal right to stay where they do, but the Indian government does not have the capacity or incentive to kick them out. Many of these homes are built near each other so that residents can share walls or watch out for each others’ property. They are also small because there is not that much free space and a lot of people competing for it. It is common to see a family of 6-8 people living in a 10’ x 10’ room! As migrants earn money, they slowly improve their homes, but it is a slow process. Importantly, the city provides very few amenities – because these individuals and their families are living on the land illegally. That means people have to pool resources to get a water tap or toilet installed, and they often share these facilities. Recently the government had a national campaign to build more toilets. But for slums, these were communal toilets because the homes were too small to install private toilets. Often you will find 4-5 toilets being shared by 100 or 200 people!
This affects a lot of people in India. More than 100 million people, roughly 25% of all urban residents in India, live in slums. In some cities, like Mumbai, 40% or more of the city lives in slums. Slums have a population density about four to 10 times what the rest of the city has. So that 40% occupies about 10% of the land in Mumbai.
In March 2020, the Indian government instituted a very strict lockdown throughout the country to slow the spread of COVID-19, including in Mumbai. Can you tell us how the lockdown changed the lives of people living in the more affluent parts of Mumbai relative to the people living in the Dharavi slums?
The lockdown had a worse impact on slums than on non-slums.
There is no question that lockdown was not pleasant outside of slums. Cities are known for small living quarters. But lockdown likely reduced the amount of human interaction in non-slum communities. In these relatively better-off areas, can reasonably segregate from other families.
But, inside slums, even that is not possible. While the probability of transmission from one household member to another in the west can be a low as 0.2, it is likely much greater in slums because everyone is always in the same room. On top of that, homes in slums have no ventilation; there is no HVAC system. These are, at best, concrete rooms. So everyone is breathing everyone else’s air without filtration. Second, a hundred or more people may share a toilet block. People have to go to the bathroom even during the lockdown. So while, in non-slums, a person may just interact with the four other people in a typical 5-person Indian family, in a slum, you will interact with dozens each time you go to the shared bathroom. On top of that, there are visits to communal water taps. Third, walking down a pathway in a slum is not like walking down the street. Because these are informal communities where people are trying to use every inch of space, pathways between homes may be just two shoulder widths wide – some smaller.
Indeed, it is possible that lockdown increased the number of people slum residents interacted with on a typical day. On a typical day, a person may leave to go to school or work. During that period, they would experience the same level of interaction with others that non-slum residents typically experience. The real crowding happens when they come home. But lockdown kept slum residents at home all day, meaning they experienced maximum density all day, not just at night.
Can you walk us through the main findings of your seroprevalence study?
Our topline result was that we found that by as early as July, slums had seroprevalence rates that were three times greater than non-slums.
Let’s dig into the details a bit. To conduct our survey, we picked three wards from each of the three regions of the city (the old city, the western suburbs and the eastern suburbs). In each ward, we selected slums and non-slums and randomly sampled within those locations. (For slums, we picked the largest slums and then selected random points within the slum to begin going door-to-door to ask people to get tested. For non-slums, we selected spots that were non-slums and evenly spaced around the ward and then went door-to-door.) We conducted this survey two times, once in July and once in August.
How widely had COVID spread through Mumbai and through the Dharavi slums?
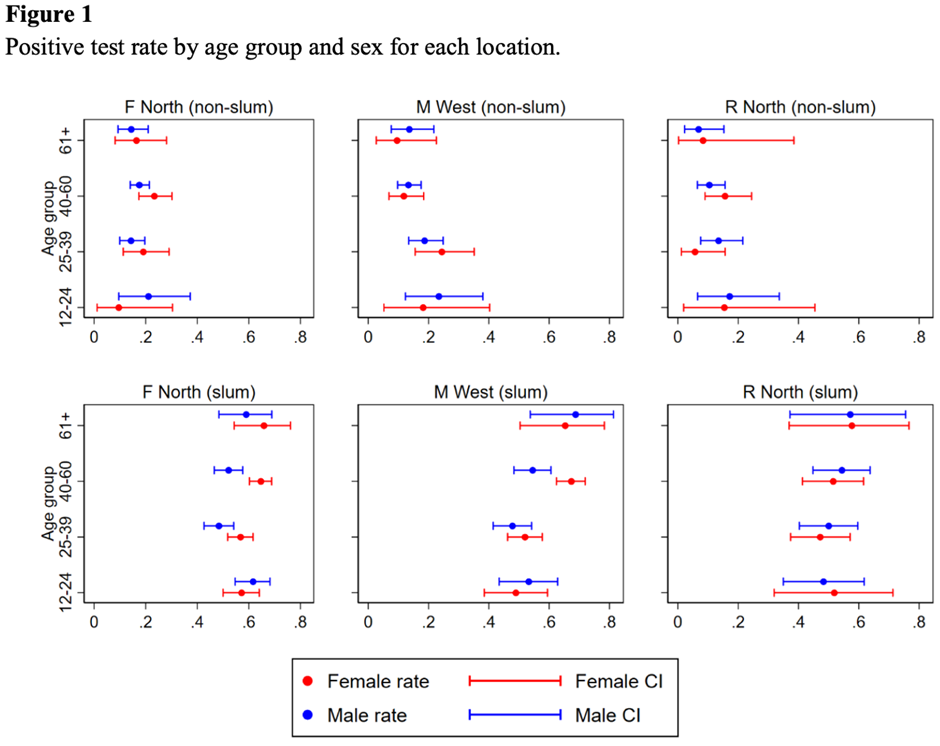
Our lab results from July suggested that 58% of individuals in slums and perhaps just 17% of individuals in non-slums had antibodies to COVID-19. (Table 1) There were no clear patterns by age or gender: people were roughly equally affected. (Figure 1)
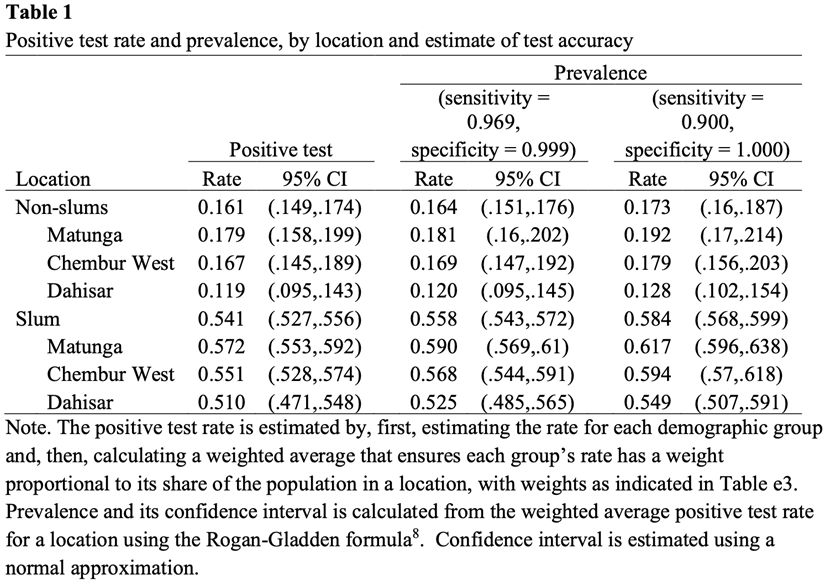
When we repeated our survey in August, we found similar numbers. The rate in slums had fallen a few percentage points, and the rate in non-slums increased a few percentage points. This was surprising because the city was reporting more cases in both types of communities.
Will you explain why the seroprevalence might be lower a month later following more infections?
To understand what was going on, it is important to know that when the body is done clearing the infection, it stops producing new antibodies and clears away old antibodies. This can take some months. If you test during those few months, you will spot the antibodies and know they were infected. But if you come too late, the antibodies will be gone.
The fact that the city was reporting cases between the two surveys, but we did not see an increase in the fraction of folks in slums with antibodies suggest that many people in slums were affected early in the pandemic. Moreover, it suggests that our seroprevalence estimates probably underestimate the fraction of people that were previously infected. Although the 58% number was high, the fraction of people previously infected may have been higher still!
What was the COVID-19 IFR in Mumbai and the Dharavi slums over that time period, and how does it compare to the IFR in the US or the UK?
We combined the city’s data on deaths in slum and non-slum areas with the results of our survey and estimated an overall infection fatality rate of 0.12%, far lower than the numbers found in developed countries at the time of the study. More recent studies have found lower estimates of IFR even in developed countries. But even the new numbers suggest the average is lower in Mumbai.
Why do you think the survival rate from the disease is higher in India than it has been in Europe and the Americas?
The top reason is probably differences in the age distribution. The average person in India and in Mumbai is much lower than the average person in the US or UK. Surveys of IFR across developed countries have found that the IFR increases exponentially with age. (It is remarkably log-linear in age.) In a subsequent paper, we plotted the IFR by age based on our data from Mumbai and found a similar relationship between age and IFR in India. We also found that there was not a tremendous gap between the IFR-age curve in Mumbai and in surveys in developed countries. The gap was 2-3x at low ages and perhaps 10x at the highest ages. This suggests age is probably the leading cause of low IFRs in India. (See Figure 1 below)
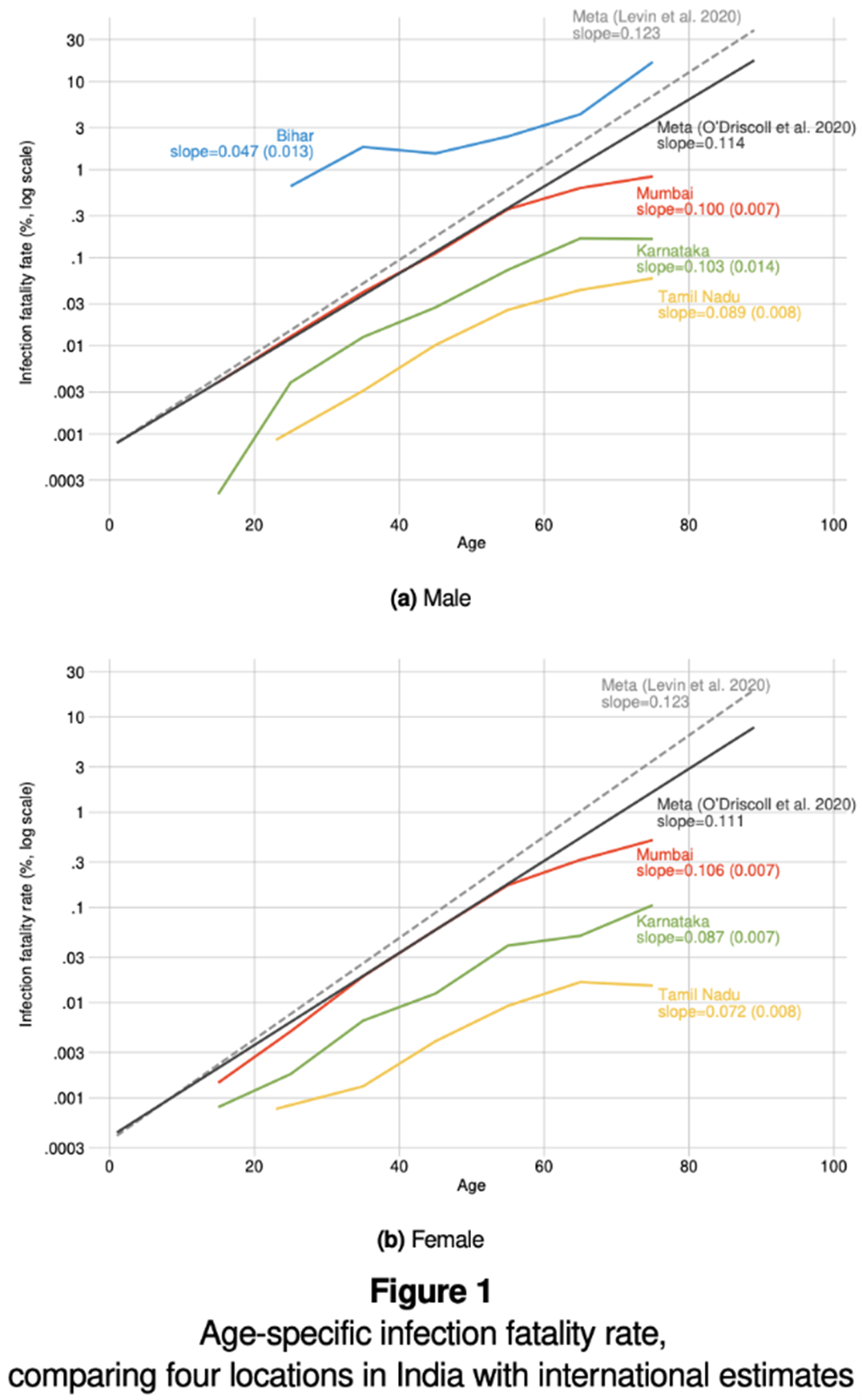
It should be noted that our estimate may be too low because the government may underestimate the number of deaths. However, Mumbai is one of the more financially wealthy cities in India and has one of the better death registries. So we do not think the undercount is massive, especially during a period where the numbers of deaths were not overwhelming facilities, like they may have done during the second wave in India in March-May 2021.
Interestingly, we found that the IFR was actually higher in non-slums (0.263%) than it was in slums (0.076%), an important clue as we try to figure why the death rate is lower in India than in higher-income countries. This finding is consistent with the idea that a high disease burden (unfortunately) killed off individuals with weaker immune systems before COVID could do so. (The non-COVID disease burden is higher in slums than non-slums.)
Did the lockdowns successfully suppress the spread of the disease in the Dharavi slums?
Again, I can speak more broadly about slums than about Dharavi, but I do not believe lockdowns were effective in suppressing the spread of COVID in slums. While lockdown may have decreased the average number of interactions non-slum residents had in a typical day, it might actually have increased the number of interactions slum residents had each day.
What might explain why the disease spread so widely despite the lockdowns?
In New York and Santiago, it has been shown that lockdowns may not have been as effective in poorer neighbourhoods because they had a smaller effect on the mobility of residents in those neighbourhoods. In the US, for example, it is thought that poorer individuals were more likely to be essential workers who were exempt from lockdowns. However, I do not believe this explanation for why lockdowns did not suppress COVID applies in slums. In work with Ashish Goel and Jaymee Sheng at Stanford and Puu Botla at Infinite Analytics, we examined the mobility of slum residents and non-slum residents based on their cell phone locations. We did not see meaningful differences in their patterns of mobility before our serological survey.
What effect did the lockdowns have on the ability of the people living in the Dharavi slums to work, feed their families, or provide a good education for their children?
I did not directly study this. However, in the last few years, I have gotten to know several NGOs working in slums around the country, and we kept in touch during the lockdown. What I heard was that food shortages were a serious problem. Schools closed, so kids lost a year of education. This was particularly saddening because education is a critical path to social mobility for new migrants. The stress of lockdown seems to have induced, at least anecdotally, an increase in the incidence of domestic violence and depression. Finally, one large pattern that we observed from NGOs, news reports and from our efforts to conduct serological surveys in slums is that a lot of residents fled the city to escape the lockdown. Our worry is that this may have spread the disease from the city to rural areas.

Anup Malani is a health & development economist and law professor at the University of Chicago and author of The Seroprevalence of SARS-CoV-2 in slums vs. non-slums in Mumbai, India.
Collateral Global encourages the republishing of all CG content not specifically designated as ‘Unavailable for Republishing’. Please see our Republishing Policy for specific requirements.
Any content is provided for your general information purposes only and to inform you about [publicly available information relating to COVID-19 and various government level strategies for addressing the pandemic provided by researchers and other third-party websites that may be of interest], but has not been tailored to your specific requirements or circumstances. It does not constitute technical, financial or legal advice or any other type of advice and should not be relied on for any purposes. You should always use your own independent judgment when using our site and its content.

