Collateral effects of lockdown to combat the COVID-19-pandemic in Austria
Andreas Sönnichsen, MD
Download full article here
Background
In March 2020 the Austrian chancellor Sebastian Kurz proclaimed that within weeks “everybody will have a family member or good friend dead due to COVID and Austria will face the horror of tens of thousands of deaths”. With these statements Austria went into lockdown on March 16, 2020, including a complete closure of all stores except supermarkets, pharmacies and banks, complete school closures and complete curfew – with few exceptions like personal emergencies.
Nobody in the administration carried out a critical assessment of possible adverse effects of lockdown or balanced benefits against risks. Critical voices, like a statement of the German Network for Evidence Based Medicine [1], were at best ignored, when they were not discredited as statements of “COVID-deniers”.
Nevertheless, it became clear quite soon that the collateral damage of the lockdown probably far outweighed the benefits, although studies and data from Austria are scarce. In this article I will present the currently available research on collateral effects of the COVID lockdowns in Austria in 2020 and 2021.
Effects of the lockdown on primary and outpatient care
The lockdown of March 16, 2020 led to an abrupt and extraordinary decline in outpatient medical consultations. During the lockdown weeks (calendar weeks 12-20) the number of curative consultations (all medical specialties together) dropped by 33.6%, and preventive consultations (cancer screening, health checks) by 61.3% compared to the same time frame in 2019. Table 1 shows the total decline, and the decline for the most widely used medical specialties for the first 26 calendar weeks of 2020 compared to 2019. The decline was most pronounced in physical therapy, radiology and traumatology. On the other hand, the number of consultations in two specialties increased: In general psychiatry and pediatric psychiatry (virtual and in person combined) the number of outpatient consultations increased by 15.9% and 10.3%, respectively, during the first 26 weeks of 2020 compared to 2019.
Fig. 1 (a-c) and Fig. 2 (a-b) depict the decline graphically compared to 2019. Fig. 3 (a-b) shows the increase in psychiatric consultations [2].
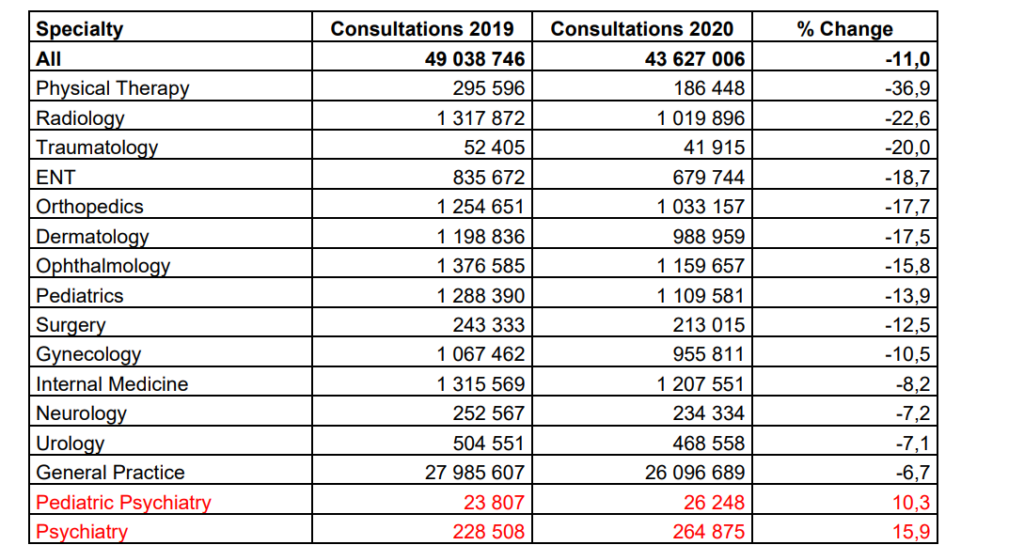
Table 1: Total number of consultations in the first half year of 2019 and 2020 in various medical specialties*
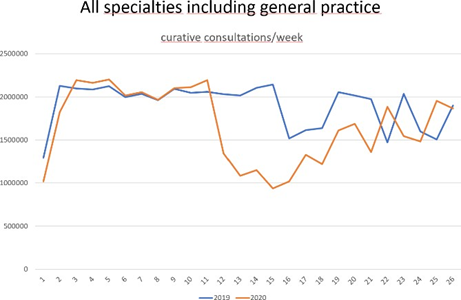
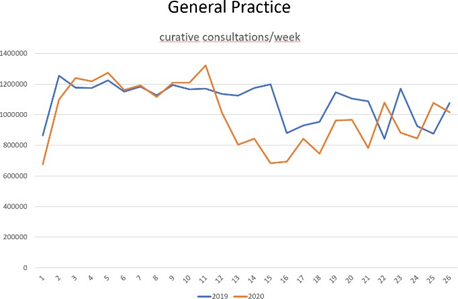
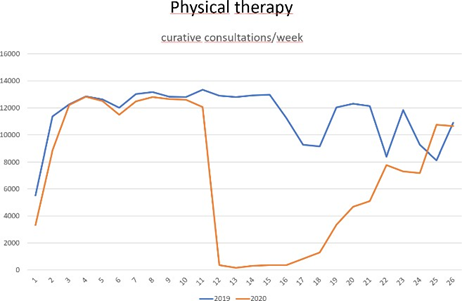
Fig.1: Curative consultations during calendar weeks 1-26 in 2019 and 2020. Data provided by ÖGK (Austrian statutory health insurance).
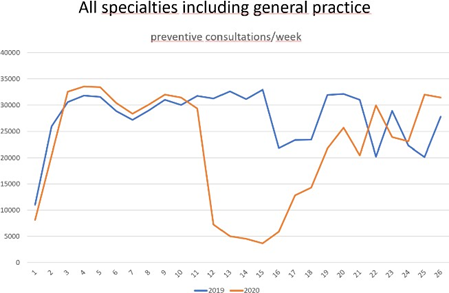
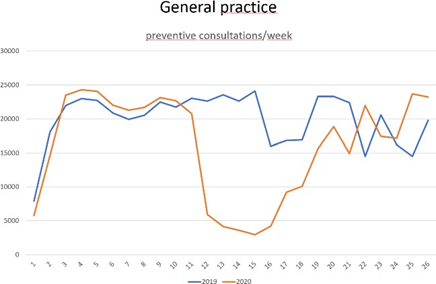
Fig. 2: Preventive consultations during calendar weeks 1-26 in 2019 and 2020. Data provided by ÖGK (Austrian statutory health insurance).
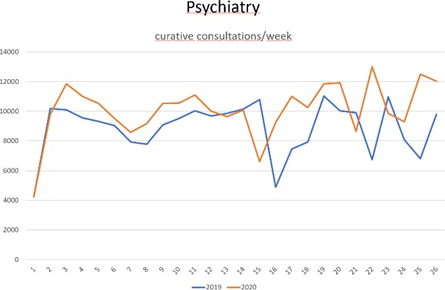
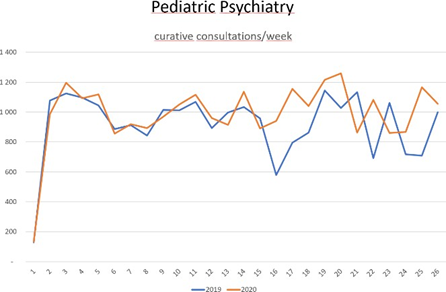
Fig. 3: Psychiatric consultations during calendar weeks 1-26 in 2019 and 2020. Data provided by ÖGK (Austrian statutory health insurance).
There are no data or studies on the effects of the decline in consultations on population or individual health in Austria. During lockdown the population was advised to stay at home and many people were afraid to leave their home for fear of getting infected. The reduction of curative consultations thus surely has led to deficits in acute medical care. The observed decline in hospital admissions for acute coronary syndromes and stroke paralleled by an increase in severity of cases supports this assumption [3]. The especially large decrease in physical therapy most likely contributed to an increase in burden from pain and physical impairment, at least temporarily. Unfortunately, in Austrian outpatient care diagnoses are not coded. Therefore, it is not possible to use insurance data to investigate lockdown effects on the frequencies of diagnoses.
Effects of the lockdown on hospital care
One of the most important reasons for the lockdown was the fear of policymakers that the pandemic would cause a capacity overload of the health care system and especially the hospitals and intensive care units. Except for some local shortages of hospital beds which are not unusual during the winter months, this never happened.
During the first pandemic wave, COVID-19 utilization of hospital beds reached a maximum of 2.0% (857 PCR-test-positive patients [4], 42 251 available acute care hospital beds in Austria [5]) in March 2020 and a maximum of 9.4% (3 985 cases) during the second pandemic wave in November 2020, and never rose above this mark during the subsequent waves. Intensive care unit utilization reached a maximum of 10.1% (267 PCR-test-positive patients [4], 2 635 available ICU-beds [6]) in March 2020 and a maximum of 26.9% (709 cases) in November 2020, a height not reached again in subsequent waves. It must be noted that these case counts do not differentiate as to whether a patient was hospitalized because of COVID-19 or hospitalization was due to another reason and the patient only had a positive PCR- test (with or without symptoms of COVID-19). This distinction is not recorded by the hospitals.
Fig. 4 shows hospital and ICU utilization during the pandemic from 1.4.2020 to 8.5.2022. Data before April 1, 2020 are not available [4].
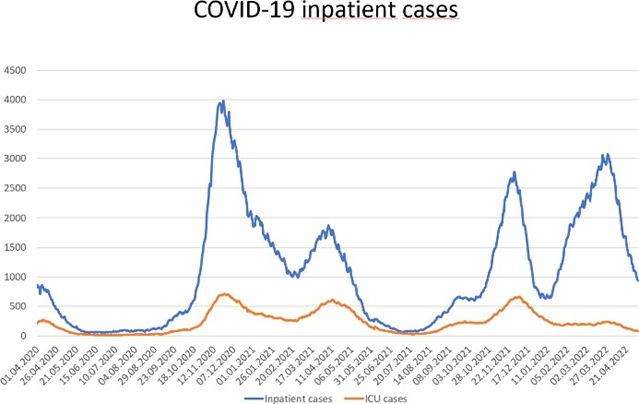
Fig. 4: Hospital and ICU utilization in Austria from 1.4.2020-8.5.2022. Data provided by AGES [4]
In total, acute hospital bed utilization decreased from 2 390 825 patients in 2019 to 1 980 489 patients in 2020 (-17.2%), and the number of performed medical procedures (surgical and non-surgical) declined by 11.7% (surgical -14.4%) [7].
As seriously ill people were not going to the hospital, they were not receiving the medical care they needed. A retrospective survey of 17 public primary percutaneous coronary intervention centres revealed that the lockdown led to a reduction of almost 40% in hospital admissions for acute coronary syndrome [3]. The authors attribute this reduction to the strict instructions to stay at home, to a misinterpretation of coronary symptoms by the patients and to the fear of infection in medical facilities. As it cannot be that the number of cardiovascular events decreased by 40% during lockdown, it is obvious that a number of affected patients did not receive adequate medical care. Metzler et al. hypothesize that the first two weeks of the lockdown may have caused 110 additional cardiovascular deaths while in the same time frame there were only 89 COVID-19-deaths in Austria. While the absolute number of patients diagnosed with acute coronary syndrome decreased, the severity of the diagnosed cases increased. A Magnetic Resonance Imaging study demonstrated that during lockdown infarct sizes increased significantly compared to pre-pandemic times [8].
Similarly, inpatient treatment of cancer decreased by about 20% during the first lockdown in March 2020 and a little less during the second and third pandemic waves from November 2020 to February 2021. Breast cancer surgery decreased from a normal level of about 500 surgeries/month to less than 350/month in May 2020 [9]. The are no data on whether the decrease in treatment had a clinical impact, but it seems inevitable that it may have led to tumor progression and a worsening of prognosis at least in some cases.
Psychological effects
While consultations in outpatient psychiatry increased by 15.9% (see above), psychiatric hospital admissions declined by about 50% during April 2020 compared to 2019. The decrease was less pronounced during the second pandemic wave.
Overall, there were 80 306 inpatient-cases with a psychiatric primary diagnosis in 2020 compared to 95 376 in 2019 (-15.8%). Considering the increase in psychiatric outpatient care and the probable increase in psychiatric disease burden due to lockdown and other measures to combat COVID (e.g., the psychological effects of the public panic initiated by policymakers and the medical community), it may be assumed that psychiatric care was inadequate in 2020.
A survey performed by the Department of Psychiatry of the Donau-University Krems on a representative sample of the Austrian population revealed a 3 to 5-fold increase in anxiety-disorders, depression and sleep-disorders in April 2020 compared to before the lockdown. 21.0%, 19.0%, and 15.7% of the population showed symptoms of moderate or severe depression, anxiety and insomnia [10]. The situation did not improve in a follow-up-survey in June 2020 [11], implying that the psychosocial effects of lockdowns persist even after a lockdown has been terminated.
A survey of more than 5 000 children carried out between February and April 2021 (during the second lockdown in Austria) showed 49% of children between 6 and 18 experiencing anxiety due to the current situation, the lockdown and the frightening information conveyed by parents and media [12]. 48.1% of the children surveyed were afraid that parents or siblings might die from COVID. When they were asked how many of 1000 healthy children of their own age would be hospitalized for COVID within one year, the children estimated between 12 (6–10-year-olds) and 33 (11–14- year-olds) while their true risk would be less than 1 in 40000. Thus, children overestimated the risk of severe COVID in healthy children by a factor of more than 100. More than 70% of the children indicated that they feel generally worse than before the pandemic, 58.2% feel angry, 46% feel lonely, and 42.7% feel depressed.
Overall, data about the psychosocial effects of lockdowns in Austria are scarce, but the few data we have are alarming, and we as yet know very little about long-term effects.
Economic effects
The total economic damage in Austria caused by the Corona-crisis is estimated to exceed 70 billion € for the years 2020-2022. About half of this amount is due to governmental aid to companies and citizens who were affected by measures taken to combat the pandemic [13]. It is difficult to distinguish between costs due to the pandemic and the disease (health care costs, economic loss due to sick leave and quarantine) and costs caused by lockdown and other countermeasures. It is even more difficult to measure cost effectiveness. It is unknown whether the costs induced by lockdown led or will lead to overall savings by preventing hospitalization or long COVID.
There are no Austrian studies estimating the effects of the lockdown on the pandemic or the economy, but international studies suggest that collateral damage could be considerably larger than the benefit. A recent meta-analysis of real life studies showed that the effect of lockdowns on the death toll is minimal to non-existent [14]. A British modelling study from 2020 estimated that the cost per QALY gained necessary to justify continuing lockdown in the UK would be £220 000 in the best- case scenario and £3.7 million in the worst-case scenario (7 and 125 times the NICE* guideline of £30 000 per QALY gained, respectively) [15]. This would mean that with lockdown, society is paying a lot more per QALY than it is willing to pay in regular medical care.
Unemployment
Austrian unemployment rose from an average of 7.4% in 2019 to a peak of 12.7% in April 2020 due to the lockdown which started on March 16, 2020. It decreased during the summer months to 8.4% and rose again to 11.4% during the second lockdown in the winter 2020/2021 [16]. In addition, many employees were working reduced working hours during lockdown. The number of employees on reduced hours went up to more than 1.2 million in May 2020 and rose to 500.000 again during the second lockdown in February 2021. In the winter of 2021/2022 there were still almost 200.000 employees on reduced hours, and numbers have returned to near zero during the summer of 2022.[17] The rise in unemployment and short-term work are for the largest part due to the measures taken against the pandemic and not the pandemic itself.
A large German national health survey investigating the effect of unemployment on life expectancy estimates that one percentage point increase in unemployment leads to an average loss in life expectancy of one month for women and three months for men [18]. It may therefore be assumed that the lockdown caused a large loss of life years, especially for the less privileged part of the population which was affected most by the rise in unemployment.
Effects of school closure
In Austria, as a measure against the pandemic, schools were completely or partially closed for 39 weeks (about 9 months) in total between March 2020 and June 2021, compared to a median of 32.5 weeks in the European Union and to only six weeks in Switzerland [19]. With more than 100 days of complete closure, upper secondary general education was affected most [20]. Although distance learning was established in most schools to compensate for school closure, learning time was probably reduced significantly. According to a German study which may be extrapolated to Austria which has a very similar school system, learning time was reduced by 3.8 hours per day on average [21]. Low achievers among the students were more affected (-4.1 hours/day). Learning time was replaced with potentially detrimental activities such as TV-watching or computer games. Especially for low- achieving students, the learning gap was in most cases not compensated by parents’ or teachers’ extra support. In short, the pandemic school closures fostered not only a loss of learning opportunities for all students but also educational inequality. There is ample literature that loss of education is closely linked to worse socioeconomic status, income, health and life-expectancy. A decision analytical model using US and European data estimated a probability of up to 98.0% that school closures will lead to more life years lost than were saved by this measure to decrease the spread of COVID [22].
Discussion
Lockdown was imposed in Austria to save lives and to prevent overload of severe COVID cases in hospitals and intensive care units. These expectations may not have been fulfilled, as it has been shown that restrictive non-pharmaceutical measures like lockdowns probably neither significantly prevent the spread of the disease [23] nor reduce mortality [14]. A thorough analysis of US-states’ differential responses to the pandemic revealed that neither lockdown nor school closures had a significant positive effect on health [24].
Emerging data point out that the negative effects of lockdown and especially school closure may outweigh possible benefits by far, leading to a net loss of life years in the population, especially in the long run. Currently, robust data regarding the detrimental effects of lockdown and school closure are scarce and only depict effects that are yet detectable. We can only hypothesize possible effects on life expectancy and mortality in the years to come. Future studies investigating these issues prospectively will enable us to further confirm the hypothesis of a negative risk-benefit-ratio.
Looking at currently available best evidence, we must advice policy makers to refrain from lockdowns and especially from school closures and to focus on alternative strategies to combat pandemics, like the targeted protection of vulnerable groups, instead of risking unprecedented harm to the whole of the population.
References
1. German Network for Evidence-based Medicine. COVID-19 – Where is the Evidence. 2020 [downloaded May 1, 2022; available from: https://www.ebm netzwerk.de/en/media/media/statement-20200323-covid-19-english.pdf/@@download]
2. Österreichische Gesundheitskasse (ÖGK – Austrian statutory health insurance). Auswertung Inanspruchnahme. Data not publicly available
3. Metzler B, Siostrzonek P, Binder RK, Bauer A, Reinstadler SJ. Decline of acute coronary syndrome admissions in Austria since the outbreak of COVID-19: the pandemic response causes cardiac collateral damage. European Heart Journal 2020;41:1852–3.
4. Agentur für Gesundheit und Ernährungssicherheit. AGES Dashboard COVID 19. 2022 [downloaded May 1, 2022; available from: https://covid19- dashboard.ages.at/dashboard.html]
5. Bundesministerium für Soziales, Gesundheit, Pflege und Konsumentenschutz. Krankenanstalten in Zahlen – tatsächlich aufgestellte Betten. 2022 [downloaded May 1, 2022; available from: http://www.kaz.bmg.gv.at/fileadmin/user_upload/ Betten/2_T_Betten_TBETT.xlsx]
6. Statistik Austria. Betten und Bettennutzung in den Krankenanstalten Österreichs 2020. [downloaded May 1, 2022; available from: http://www.statistik.at/wcm/idc/idcplg?IdcService= GET_NATIVE_FILE&RevisionSele ctionMethod=LatestReleased&dDocName=022343]
7. Prammer-Waldhör M, Klimont J. Jahrbuch der Gesundheitsstatistik 2020. 2022 [downloaded May 1, 2022; available from: http://www.statistik.at/wcm/idc/idcplg?IdcService=GET_NATIVE_FILE &RevisionSele ctionMethod=LatestReleased&dDocName=127965]
8. Lechner I, Reindl M, Tiller C, Holzknecht M, Troger F, Fink P, u. a. Impact of COVID-19 pandemic restrictions on ST-elevation myocardial infarction: a cardiac magnetic resonance imaging study. European Heart Journal 2022;43:1141–53.
9. Eglau K. Auswirkungen der COVID‐19‐ Pandemie auf die stationäre Spitalsversorgung anhand ausgewählter Bereiche. 2021 [downloaded May 1, 2022; available from: https://jasmin.goeg.at/1633/1/Auswirkungen% 20COVID19_KA_Aktualisierung_Gesa mtjahr2020_bf.pdf]
10. Pieh C, Budimir S, Probst T. The effect of age, gender, income, work, and physical activity on mental health during coronavirus disease (COVID-19) lockdown in Austria. Journal of Psychosomatic Research 2020;136:110186.
11. Probst T, Budimir S, Pieh C. Depression in and after COVID-19 lockdown in Austria and the role of stress and loneliness in lockdown: A longitudinal study. Journal of Affective Disorders 2020;277:962–3.
12. Schabus M, Eigl ES. [“Now You’re Talking!”]. Padiatr Padol 2021;56:170–7.
13. Prettner K. Was hat Corona bis jetzt den österreichischen Staat gekostet? 2022 [downloaded May 1, 2022; available from: https://www.wu.ac.at/other/zukunftsperspektiven-nach-der-coronakrise-1/ corona-qa details/detail/was-hat-corona-bis-jetzt-den-oesterreichischen-staat-gekostet]
14. Herby J, Jonung L, Hanke S. A Literature Review and Meta-Analysis of the Effects of Lockdowns on COVID-19 Mortality. 2022 [downloaded May 1, 2022; available from: https://sites.krieger.jhu.edu/iae/files/2022/01/ A-Literature-Review-and Meta-Analysis-of-the-Effects-of-Lockdowns-on-COVID-19-Mortality.pdf]
15. Miles D, Stedman M, Heald AH. “Stay at Home, Protect the National Health Service, Save Lives”: a cost benefit analysis of the lockdown in the United Kingdom. Int J Clin Pract 2020 [downloaded May 1, 2022; available from: https://onlinelibrary.wiley.com/doi/abs/10.1111/ijcp.13674]
16. Arbeitsmarktservice. Arbeitsmarktdaten online. 2022 [downloaded May 1, 2022; available from: https://iambweb.ams.or.at/ambweb/]
17. Statista. Employees on reduced hours in Austria 2020-2022. 2022 [downloaded Jan 9, 2023; available from: https://de.statista.com/statistik/daten/studie/1198022/ umfrage/kurzarbeiter-in oesterreich/]
18. Kroll L, Lampert T. Arbeitslosigkeit, prekäre Beschäftigung und Gesundheit. Hrsg. Robert-Koch-Institut, GBE kompakt, Berlin 2012 [downloaded Apr 1, 2022;. available from: https://www.rki.de/DE/ Content/ Gesundheitsmonitoring/Gesundheitsberichterstattung/ GBEDownloadsK/2012_1_Arbeitslosigkeit_Gesundheit.html?nn=2532006]
19. Bock-Schappelwein J, Famira-Mühlberger U. Ausmaß und Effekte von Schulschließungen. Österreich im internationalen Vergleich. 2021 [downloaded May 1, 2022; available from: https://www.wifo.ac.at/jart/prj3/ wifo/resources/person_dokument/person_dokument.ja rt?publikationsid=69247&mime_type=application/pdf#:~:text= g%C3%A4nzlichen%20 Schulschlie%C3%9Fungen%20in%20der%20EU,Zeit%20 teilweise%20oder%20g%C 3%A4nzlich%20geschlossen]
20. OECD. The State of Global Education: 18 Months into the Pandemic. 2021 [downloaded May 7, 2022; available from: https://www.oecdilibrary.org/education/the-state-of-global-education_1a23bb23-en]
21. Grewenig E, Lergetporer P, Werner K, Woessmann L, Zierow L. COVID-19 and educational inequality: How school closures affect low- and high-achieving students. European Economic Review 2021;140:103920
22. Christakis DA, Van Cleve W, Zimmerman FJ. Estimation of US Children’s Educational Attainment and Years of Life Lost Associated With Primary School Closures During the Coronavirus Disease 2019 Pandemic. JAMA Netw Open 2020;3:e2028786
23. Bendavid E, Oh C, Bhattacharya J, Ioannidis JPA. Assessing mandatory stay‐ at‐home and business closure effects on the spread of COVID‐19. Eur. J. Clin. Invest. 2021;51:e13484
24. Kerpen P, Moore S, Mulligan CB. A Final Report Card on the States’ Response to COVID-19. 2022 [downloaded May 1, 2022; available from: http://www.nber.org/papers/w29928]
